Prominent CNM Educator to Launch Rwanda’s First Master’s in Midwifery Program
Pamela Meharry, PhD, CNM, RN, first arrived in Rwanda in 2015, part of an ambitious initiative to train the healthcare workforce in the post-genocide country in east Africa.
She was there to co-teach in the newly created Bachelor of Science in midwifery program at the University of Rwanda.
But in a short time, Meharry saw a need for more than a bachelor’s program, envisioning an advanced degree where midwifery leaders could be cultivated on Rwandan soil.
“The midwives I taught with had either gone abroad to Australia, Canada, Scotland, South Africa, or Uganda for their midwifery master’s degree, or completed a master’s program in another discipline,” she says. “When I first started talking about a master’s in midwifery, [my colleagues] said, ‘you’ll have 50 people signed up on day one to join that class. So many midwives wanted to do it, but there was no program.”
Following years of planning with other stakeholders, Meharry’ s vision will become a reality in April, when the inaugural class of students will begin in the Master of Science in midwifery program at the University of Rwanda.
Reducing mortality rates
 The University of Illinois Chicago (UIC) School of Nursing hired Meharry – who was working in Connecticut as a midwife and instructor – to travel to Rwanda under the banner of the Human Resources for Health Program, the largest U.S. academic global health consortium to date.
The University of Illinois Chicago (UIC) School of Nursing hired Meharry – who was working in Connecticut as a midwife and instructor – to travel to Rwanda under the banner of the Human Resources for Health Program, the largest U.S. academic global health consortium to date.
During the Rwandan genocide in 1994, an estimated 800,000 people were killed, and the small nation faced a severe shortage of qualified physicians, nurses, midwives, and other healthcare workers. UIC Nursing was one of five U.S. nursing schools selected to participate in the program.
Meharry was paired with the head of the midwifery department and co-taught bachelor’s degree and master’s degree students in the neonatal nursing program, but she observed that a master’s in midwifery program was also sorely needed to develop teachers and leaders.
There were eight other masters’ programs in the School of Nursing and Midwifery at the University of Rwanda, though none that specialized in midwifery or women’s health.
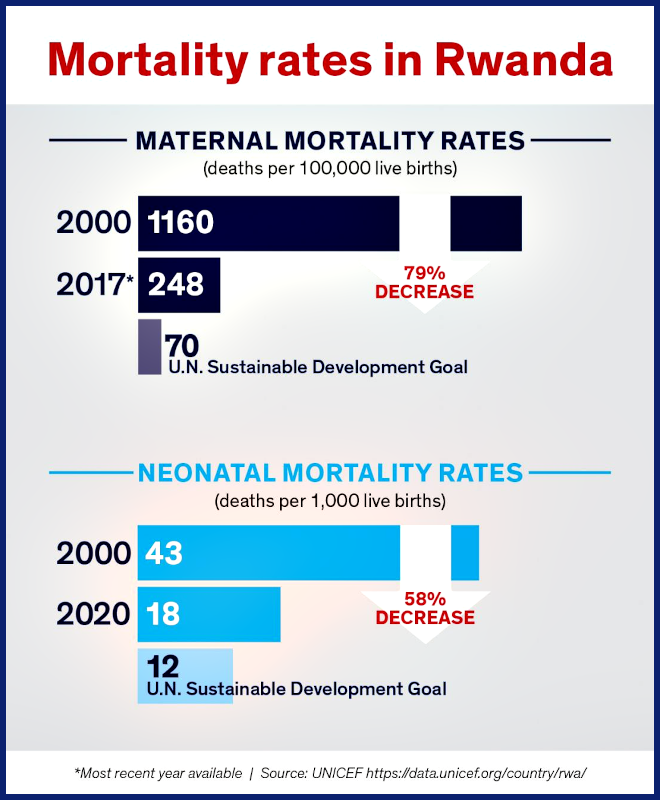
She adds that midwives are considered vital assets in the global effort to lower maternal and infant mortality rates. In Rwanda, those rates have decreased significantly over the last 20 years, but there is more work to be done to reach U.N. Sustainable Development Goals by the benchmark year of 2030, she says.
UIC Nursing shares curriculum
With permission from her Rwandan department head to begin pulling together a curriculum, Meharry contacted UIC Nursing’s then-associate dean for global health Linda McCreary, PhD ’00, MS ’93, BSN ’73, RN, FAAN, and nurse-midwifery program director Carrie Klima, PhD, MS ’86, CNM, FACNM, FAAN. Those colleagues shared with her the UIC DNP nurse-midwifery curriculum, giving her a strong basis from which to develop a curriculum appropriate for a new master’s program at the University of Rwanda.
Meharry was involved in curriculum development even as she conducted a Fulbright teaching and research grant in Zimbabwe in 2019 and 2020. The new master’s program was approved in November 2021.
Meharry says this will open doors for midwives.
“At the master’s level, well-trained midwives [can] assume a leadership role in training midwives, increasing competencies and critical decision-making skills, stimulating research and publications, and integrating more evidence-based practice into health facilities,” Meharry says.
Developing research and study abroad opportunities
During her seven years in Africa, Meharry has also played a vital role in mentoring student researchers, helping 27 nursing master’s graduates publish articles in issues of the Rwandan Journal of Medicine and Health Science.
These publications have become a labor of love and significantly enhance the graduates’ prospects of promotion and PhD studies,” Meharry says. “We now have six graduates in the new PhD program, and they [recently] presented their doctoral proposals to the faculty for review.”
Meharry also helped the head of the midwifery department to publish her master’s research and is now co-supervising her PhD research.
Originally from New Zealand, Meharry says she loves Rwanda’s temperate climate and open spaces. However, what keeps her there is the opportunity to help build programs and develop a research-rich environment, which she finds very rewarding.
She’s hoping to pass that enthusiasm on to UIC Nursing students by serving as faculty director for a month-long Rwanda study abroad program in July 2022 — Global Maternal and Child Health in Rwanda – the first maternal and child health course offered by the UIC Study Abroad Office.