A1C, or Hemoglobin A1C (HbA1c), is considered the gold standard for managing diabetes. But what is it?
The cell wall of the erythrocyte is permeable to glucose. Exposed to this glucose, the Hemoglobin molecule becomes “glycated.” The naming convention for HbA1c derives from Hemoglobin type A being separated using cation exchange chromatography. The first fraction, considered the pure Hemoglobin A is designated HbA0. After that comes HbA1a, HbA1b, and then HbA1c respective of their elution. Hemoglobin exposed to a normal level of glucose has an average glycation. As the glucose level rises, so does the fraction of glycated Hemoglobin, in a predictable way.
The average lifespan of a red blood cell is about 120 days before the cell membrane starts showing signs of wear and tear and they get shuttled off to the spleen, liver, and bone marrow for breakdown and recycling. The A1C therefore is a picture of the AVERAGE blood sugar over the previous 2-3 months. As an average, it cannot tell the difference between someone with tightly controlled blood sugar and a person with wildly fluctuating highs and lows. Neither does it identify episodes of hypoglycemia or periods of critically high blood sugar values. It’s great for population management but too crude a tool to manage an individual patient.
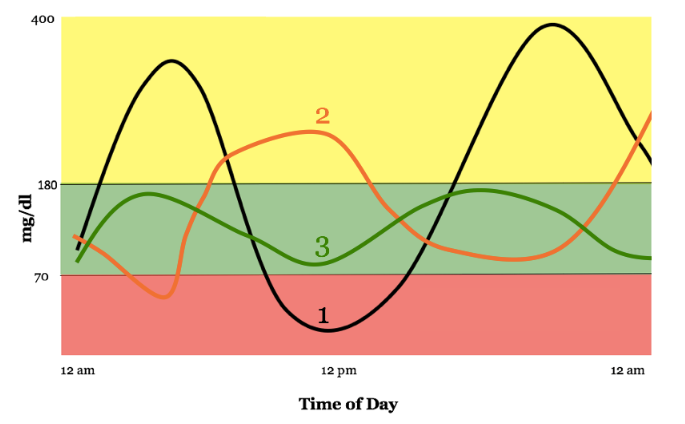 In the chart, we see a day in the blood sugar levels of three patients. All three have the same average blood sugar, but patient number 1 and patient number 2 have wildly fluctuating levels throughout the day. Patient 1 spends more time outside of range than inside, but her A1C would be normal.
In the chart, we see a day in the blood sugar levels of three patients. All three have the same average blood sugar, but patient number 1 and patient number 2 have wildly fluctuating levels throughout the day. Patient 1 spends more time outside of range than inside, but her A1C would be normal.
The A1C coupled with the patient’s daily blood sugar record gives a more complete picture for individual patient management. Other shortcomings in the A1C happen with patients with high or low blood cell turnover. Patients with kidney disease undergoing dialysis have especially high turnover of red blood cells due to the process of filtering the blood. Their A1C would be abnormally low. Cirrhosis of the liver decreases blood cell turnover leading to higher A1C levels. Certain types of anemia and blood disorders as well as some vitamins and medications can affect the accuracy of the A1C. If you hang your hat on the A1C for all your treatment decisions, you will be misled.
So, what is the A1C good for? The American Diabetes Association has the following guidelines to be used in the diagnosis of diabetes:
| A1c Level | What It Means |
| Less than 5.7% | Normal (minimal risk for type 2 diabetes) |
| 5.7% to 6.4% | “Prediabetes,” meaning at risk for developing type 2 diabetes |
| 6.5% or greater | Diagnosed diabetes |
Following it over time allows for risk evaluation for complications arising from diabetes. There’s a strong positive correlation between high A1C numbers and diabetic neuropathy, kidney disease, and eye disease. Diabetic specialists use the daily blood sugar levels to formulate an individual plan for each patient to drive the A1C numbers lower over time.
Understanding the A1C and what it does and does not tell you is important. It’s a great starting point, but not an accurate tool for individualized diabetes care.
- A Letter from the Road: A COVID-19 Crisis Nurse from San Quentin Prison Reports - September 4, 2020
- Home Health in the Time of COVID-19 - July 8, 2020
- An Occupational Health Nurse’s First Day - February 24, 2020