I’m doing laundry at a wash & fold in front of the house boats of Sausalito. Reminder: buy more scrubs. I’m one mile from from the hotel. Three minutes by car, 10 minutes by bicycle. The views are great. The weather is awesome. I could live here easy. Not on a house boat though.
They have a problem with the mating calls of some kind of small mud fish whose population has exploded. I guess it sounds terrible, like hammers on the hull all night long. Nature.
The hotel is a popular national chain brand in Mill Valley, gateway to Mount Tamalpais, and Muir Woods. It’s just north of San Francisco. I can just barely see Coit Tower. I’m maybe an hour and a half from my home so the commute would be brutal. The state is picking up the hotel tab thanks to a program authorized by the governor. It’s been a godsend.
The hotel is using the pandemic money to remodel. The room is nice, but there are sawzalls and hammers and loud Mariachi music playing during the day. At least I’m hardly ever there. They don’t clean the rooms as often because of the pandemic, but you can get fresh towels and coffee pods at the front desk any time.
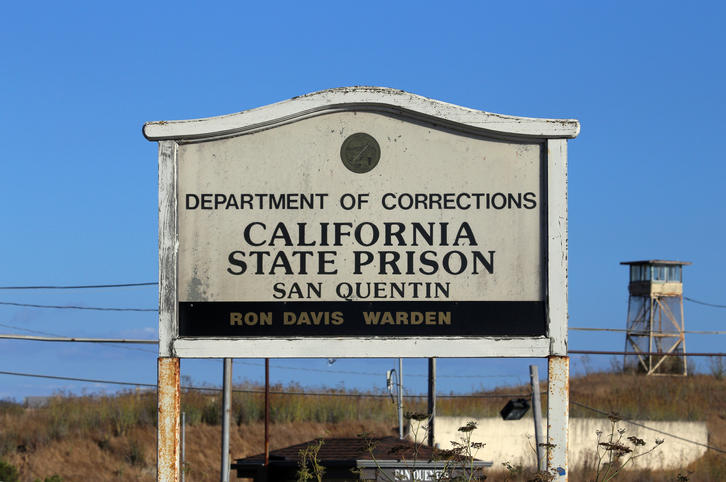
The job is tedious, but not difficult. Basically, you make rounds on the prison population two times daily trying to root out COVID patients and separate them. I get there at 5:30 AM. There is a line to get through the gate. I have to sign four different log books in four different areas plus clock in with a time card.
We got a great tour of the prison on day one. The thing I remember the most is when the nurse educator guiding us said, “To everyone else they are prisoners, to us they are patients…all of them.” This dichotomy in mandates between prison staff and medical staff has allowed me to put the job neatly into my bailiwick. Nursing is nursing. The rest of it is for prison staff to handle.
The whole prison is on lock down. It’s quiet in the yards. It’s been grim. However there is hope. The numbers are improving. On my first day, there were over 1,300 patients in isolation. Two weeks later, the number is half of that. Everyone wears a mask. Infection control is taken seriously. Teams of nurses go out twice daily to assess the inmates. Other teams are doing COVID testing. Every staff member gets tested once per week. Cautiously, things are returning to a semblance of normalcy, whatever that means in a prison.
We pair up—an RN and an LVN—and grab our shoulder bag. Inside the bag is an IR thermometer, a pulse oximeter, a BP cuff, disposable PPE, alcohol wipes…sundries. When we get to our assigned area we put on the PPE and each team gets their own guard to keep them safe. “Don’t step into the cell, don’t put your face in front of the food port, don’t walk close to the cells…” Helpful advice and a sober reminder of the overlapping existence of prisoner and patient.
I’ve given careful thought to the nature of the job, the nature of crime and punishment, and the morally ambiguous task of providing competent health care to people who have committed terrible crimes. Thankfully, I’ve never followed crime stories. Having worked in the ER for many years, I’ve dealt exclusively with the aftermath of crime and the amelioration of its physical consequences…as best as can be done anyway. I have no curiosity about death row inmates. I can honestly say that I leave that at the door and look at each person strictly through the lens of health care. Having said that, I can tell from even the most cursory interactions with some of the patients that there are some seriously disturbed people within these walls. I’m happy to move along to lower level offenders.
From the ground, I can say the efforts to control the spread of COVID within the prison have been very successful. Again, I’m just the tip of the spear so the big picture is a little out of my view. But just judging from the numbers of patients I assess daily, things are improving very quickly. I guess that’s the benefit of working within a closed system…it was also that closed system that allowed the virus to spread so quickly in the first place, so there’s that. Wearing masks, social distancing, testing, contact tracing, quarantining…they have brought the cases of infection down so quickly that it’s possible that the job will end early. I’ll be sorry to leave. The pay is…generous.
The best part of the experience has been meeting new friends. Travel nurses are go-getters. I’ve met nurses from all over the world on this assignment. We share a common bond and have moved together from trepidation to confidence in this new role. We share stories in the break room and compare notes on our experience. Several nurses are staying in the same hotel that I am. It’s a great way to meet friends in our new socially isolated world. I hope that I have met lifelong friends here as I have on other contracts. The staff at the prison have been nothing but welcoming, same for my agency. A good experience from top to bottom.
The good news…or bad news depending on how you look at it, is that other prisons are experiencing similar outbreaks and will need COVID crisis teams to come in. There are already jobs being posted for other prisons in California. Susanville, San Lois Obispo, are two that I’ve seen. If you are interested in making some quick money, and are willing to shoulder some risk, I encourage you to contact a recruiter. The turnaround time for me was three days between first contact and clocking in. Be ready to move quickly. Have your documents together. The free hotel program is still in effect so your housing is covered. Stay safe out there.
- A Letter from the Road: A COVID-19 Crisis Nurse from San Quentin Prison Reports - September 4, 2020
- Home Health in the Time of COVID-19 - July 8, 2020
- An Occupational Health Nurse’s First Day - February 24, 2020